Climate Change Impact (CO₂ Equivalent)
Annual CO₂ eq emissions based on an independent study of 728,000 DIN baskets processed per year in Scotland.
Environmental Impact Study
The NHS Scotland National Green Theatres Programme commissioned a Lifecycle Analysis (LCA) and Comparative Carbon Footprint Study of Pre-Wash methods for Decontamination of Medical Devices. This research was conducted by Dr. Yan Wang, Mr. Luca Venuti, and Miss Shufei Wang at the University of Brighton. Prof Mahmood Bhutta, Professor of Sustainable Healthcare, Consultant ENT Surgeon, University Hospitals Sussex is currently preparing the paper to submit for peer reviewed publication.
Study Methodology
The research compared three different pre-wash methods for decontaminating surgical medical devices at the Central Decontamination Centre, NHS Greater Glasgow and Clyde at Cowlairs:
- Manual pre-wash (sink with warm water and detergent)
- Tiny Air automated system
- Medisafe SI PCF Ultrasonic machine
The study followed ISO14040, ISO14044 standards and the International Life Cycle Data System (ILCD) guidelines. The functional unit was the set of contaminated medical devices kept together in ½ DIN Baskets (250 x 500 mm) throughout the decontamination processes.
Environmental Impact Analysis
The study used Open LCA (Version 2.2) software and the Ecoinvent database (Version 3.10) with the EF v3.1 impact Analysis method recommended by the European Commission. Primary data was collected at Cowlairs between April to June 2024, including:
- Water consumption
- Electricity usage
- Natural gas energy for water heating
- Detergent consumption
- Waste water production
Resource Consumption Comparison
| Resource | Manual Pre-wash | Tiny Air | Ultrasonic Machine |
|---|---|---|---|
| Water Usage | 32.5 liters | 28 liters | 84 liters |
| Electricity | 0 kWh | 0.24 kWh | 1.01 kWh |
| Gas Energy (water heating) | 1.36 kWh | 0 kWh | 4.28 kWh |
| Detergent | 125 ml | 0 ml | 125 ml |
| Cycle Time | Variable | 2 minutes | 33 minutes |
| Rewash Rate | 3% | 0.93% | 3% |
Environmental Conclusion
The comparative lifecycle analyses conclusively demonstrate that different decontamination methods for reusable surgical medical devices have significantly different environmental footprints. The results show that Tiny Air's pre-wash system has substantially lower environmental impacts compared to both manual and ultrasonic machine pre-wash methods.
There are approximately 728,000 ½ DIN baskets decontaminated per year in Scotland. By implementing Tiny Air's pre-wash technology to replace conventional methods, healthcare facilities can avoid:
- 1,034 tonnes of CO₂ equivalent emissions compared to ultrasonic machines
- 230 tonnes of CO₂ equivalent emissions compared to manual pre-wash
- Significant water consumption (54 liters saved per cycle compared to ultrasonic)
- Complete elimination of detergent usage (125ml per cycle)
- Reduced energy consumption for water heating
- Lower rewash rates (0.93% vs 3% for other methods)
Sensitivity Analysis
The study also performed sensitivity analyses considering:
- Rewash Rate Impact: Even considering different rewash rates (0.93% for Tiny Air vs 3% for other methods), Tiny Air's environmental impact remains at 86% of manual wash and 50% of ultrasonic machines.
- Energy Composition: When using Scotland's renewable energy mix, Tiny Air's environmental impact decreases further to just 21% of manual pre-wash and 7% of ultrasonic pre-wash.
NHS Net Zero Goals
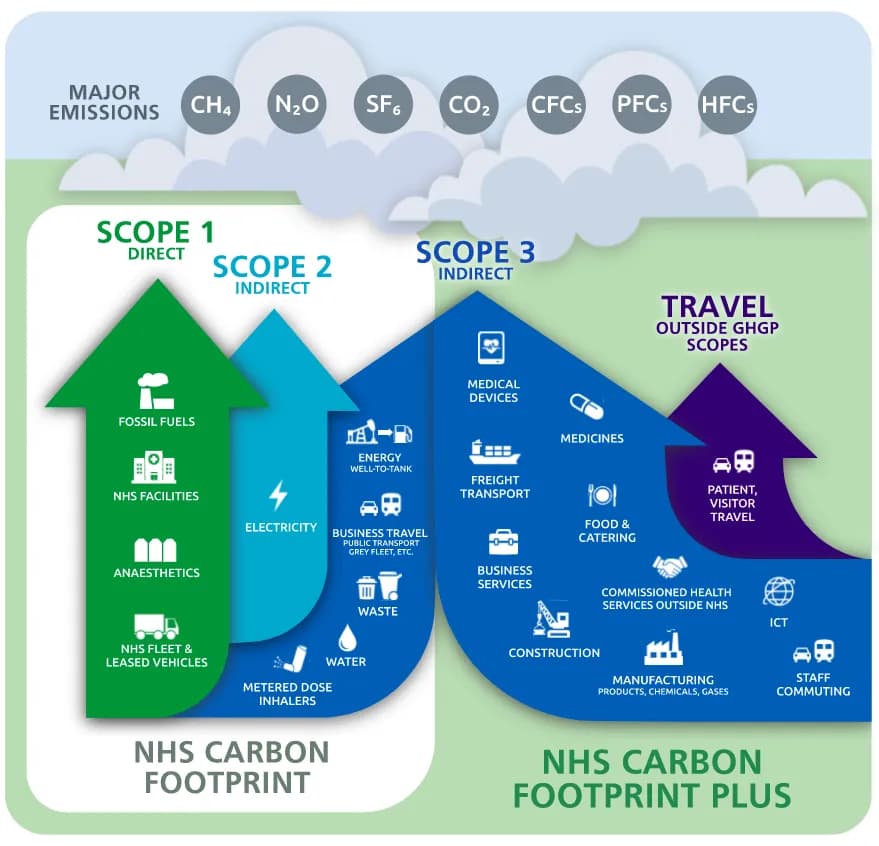
The NHS aims to reach Net Zero by 2040 for the emissions they can directly control, with an ambitious target of 80% reduction by 2028-2032, and complete net zero by 2045 for emissions they can influence.
Research has shown that the use-phase of surgical medical devices is the largest contributor to the environmental impact of reusable items, particularly during decontamination processes.